
May 22,2025 Hydronidone (F351) Phase 3 Trial in CHB-Associated Liver Fibrosis -
Topline Data Review NASDAQ: GYRE
Forward Looking Statements This presentation contains “forward-looking
statements” within the meaning of the federal securities laws regarding the current plans, expectations and strategies of Gyre Therapeutics, Inc. and its subsidiaries (“Gyre”), which statements are subject to substantial risks and uncertainties
and are based on management’s estimates and assumptions. All statements, other than statements of historical facts included in this presentation, are forward-looking statements, including statements concerning: Gyre’s plans, objectives, goals,
strategies, future events, or intentions relating to Gyre’s products and markets; the safety, efficacy and clinical benefits of Gyre’s product candidates; the anticipated timing and design of any planned or ongoing preclinical studies and
clinical trials; Gyre’s research and development efforts; timing of expected clinical readouts, including timing of initiation of Gyre’s Phase 2 trial in the U.S. for F351 for the treatment of MASH-associated liver fibrosis, timing of
completion of Gyre’s Phase 2 clinical trial in the PRC of F573 for ALF/ACLF, Gyre’s initiation of Phase 1 trial of F230 for the treatment of PAH and IND submission of F528 in COPD, the expectations regarding commercial launch of nintedanib and
avatrombopag maleate tablets, management’s plans and objectives for future operations and future results of anticipated product development efforts; potential addressable market size; and Gyre’s liquidity and capital resources and business
trends. In some cases, you can identify forward-looking statements by terms such as “believe,” “can,” “could,” “design,” “estimate,” “expect,” “forecast,” “intend,” “may,” “might,” “plan,” “potential,” “predict,” “objective,” “should,”
“strategy,” “will,” “would,” or the negative of these terms, and similar expressions intended to identify forward-looking statements. These statements involve known and unknown risks, uncertainties and other factors that could cause Gyre’s
actual results to differ materially from the forward-looking statements expressed or implied in this presentation, such as the uncertainties inherent in the clinical drug development process, the regulatory approval process, the timing of any
regulatory filings, the potential for substantial delays, the risk that earlier study results may not be predictive of future study results, manufacturing risks, and competition from other therapies or products, as well as those described in
“Risk Factors” and “Management’s Discussion and Analysis of Financial Condition” in Gyre’s Annual Report on Form 10-K for the year ended December 31, 2024 filed on March 17, 2025 with the Securities and Exchange Commission (the “SEC”) and
elsewhere in such filing and in Gyre’s other periodic reports and subsequent disclosure documents filed with the SEC. Gyre cannot assure you that it will realize the results, benefits or developments that it expects or anticipates or, even if
substantially realized, that they will result in the expected consequences or affect Gyre or its business in the ways expected. Forward-looking statements are not historical facts, and reflect management’s current views with respect to future
events. Given the significant uncertainties, you should evaluate all forward-looking statements made in this presentation in the context of these risks and uncertainties and not place undue reliance on these forward-looking statements as
predictions of future events. All forward-looking statements in this presentation apply only as of the date made and are expressly qualified in their entirety by the cautionary statements included in this presentation. Gyre has no intention to
publicly update or revise any forward-looking statements to reflect subsequent events or circumstances, except as required by law. Gyre obtained the data used throughout this presentation from its own internal estimates and research, as well as
from research, surveys and studies conducted by third parties. Internal estimates are derived from publicly available information and Gyre’s own internal research and experience, and are based on assumptions made by management based on such
data and its knowledge, which it believes to be reasonable. In addition, while Gyre believes the data included in this presentation is reliable and based on reasonable assumptions, Gyre has not independently verified any third-party
information, and all such data involve risks and uncertainties and are subject to change based on various factors. This presentation concerns a discussion of investigational drugs that are under preclinical and/or clinical investigation and
which have not yet been approved for marketing by the U.S. Food and Drug Administration. They are currently limited by Federal law to investigational use, and no representations are made as to their safety or effectiveness for the purposes for
which they are being investigated. 2
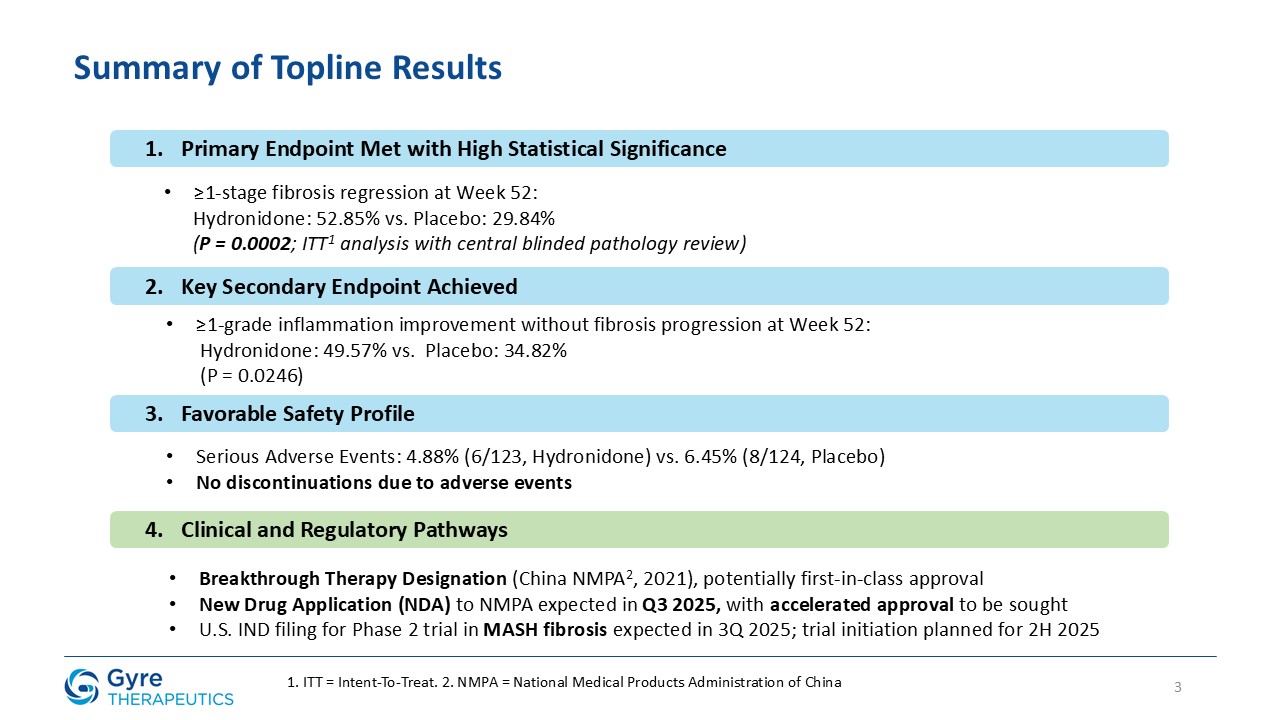
3 Summary of Topline Results Primary Endpoint Met with High Statistical
Significance ≥1-stage fibrosis regression at Week 52: Hydronidone: 52.85% vs. Placebo: 29.84% (P = 0.0002; ITT1 analysis with central blinded pathology review) Key Secondary Endpoint Achieved ≥1-grade inflammation improvement without
fibrosis progression at Week 52: Hydronidone: 49.57% vs. Placebo: 34.82% (P = 0.0246) Favorable Safety Profile Serious Adverse Events: 4.88% (6/123, Hydronidone) vs. 6.45% (8/124, Placebo) No discontinuations due to adverse
events Clinical and Regulatory Pathways Breakthrough Therapy Designation (China NMPA2, 2021), potentially first-in-class approval New Drug Application (NDA) to NMPA expected in Q3 2025, with accelerated approval to be sought U.S. IND
filing for Phase 2 trial in MASH fibrosis expected in 3Q 2025; trial initiation planned for 2H 2025 1. ITT = Intent-To-Treat. 2. NMPA = National Medical Products Administration of China
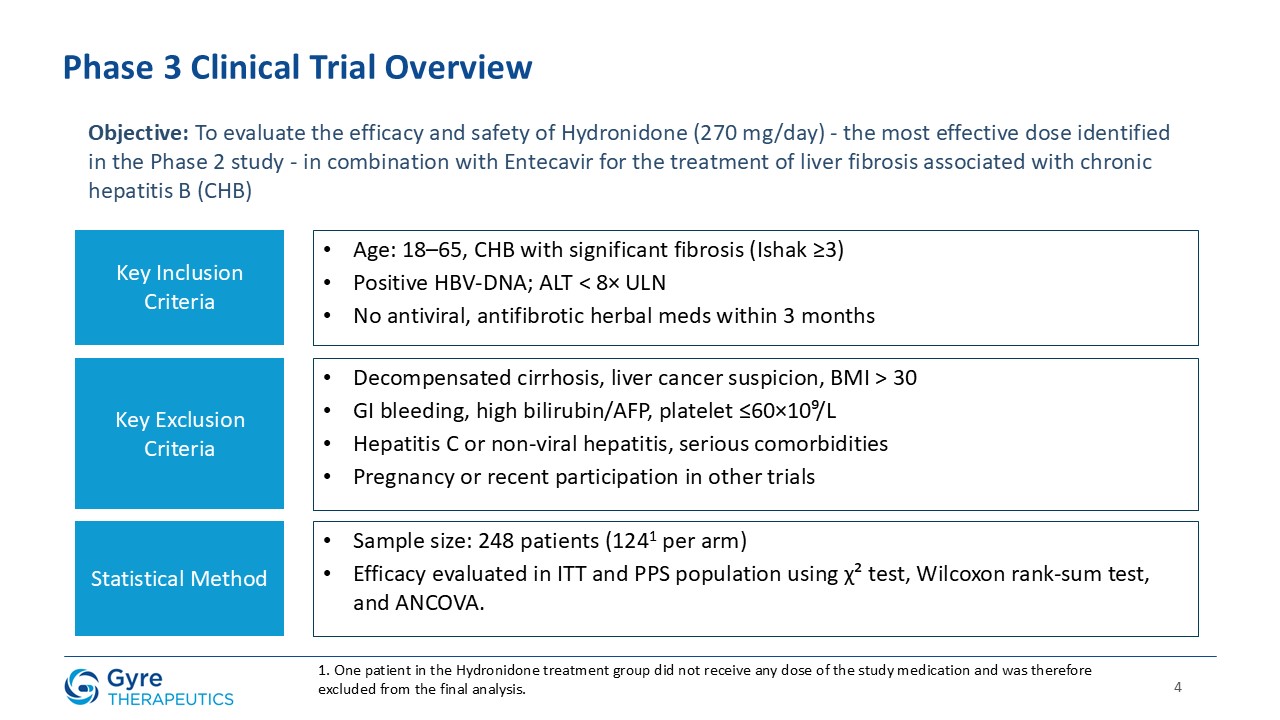
4 Phase 3 Clinical Trial Overview Objective: To evaluate the efficacy and safety
of Hydronidone (270 mg/day) - the most effective dose identified in the Phase 2 study - in combination with Entecavir for the treatment of liver fibrosis associated with chronic hepatitis B (CHB) Key Inclusion Criteria Key Exclusion
Criteria Statistical Method Age: 18–65, CHB with significant fibrosis (Ishak ≥3) Positive HBV-DNA; ALT < 8× ULN No antiviral, antifibrotic herbal meds within 3 months Decompensated cirrhosis, liver cancer suspicion, BMI > 30 GI
bleeding, high bilirubin/AFP, platelet ≤60×10⁹/L Hepatitis C or non-viral hepatitis, serious comorbidities Pregnancy or recent participation in other trials Sample size: 248 patients (1241 per arm) Efficacy evaluated in ITT and PPS
population using χ² test, Wilcoxon rank-sum test, and ANCOVA. 1. One patient in the Hydronidone treatment group did not receive any dose of the study medication and was therefore excluded from the final analysis.
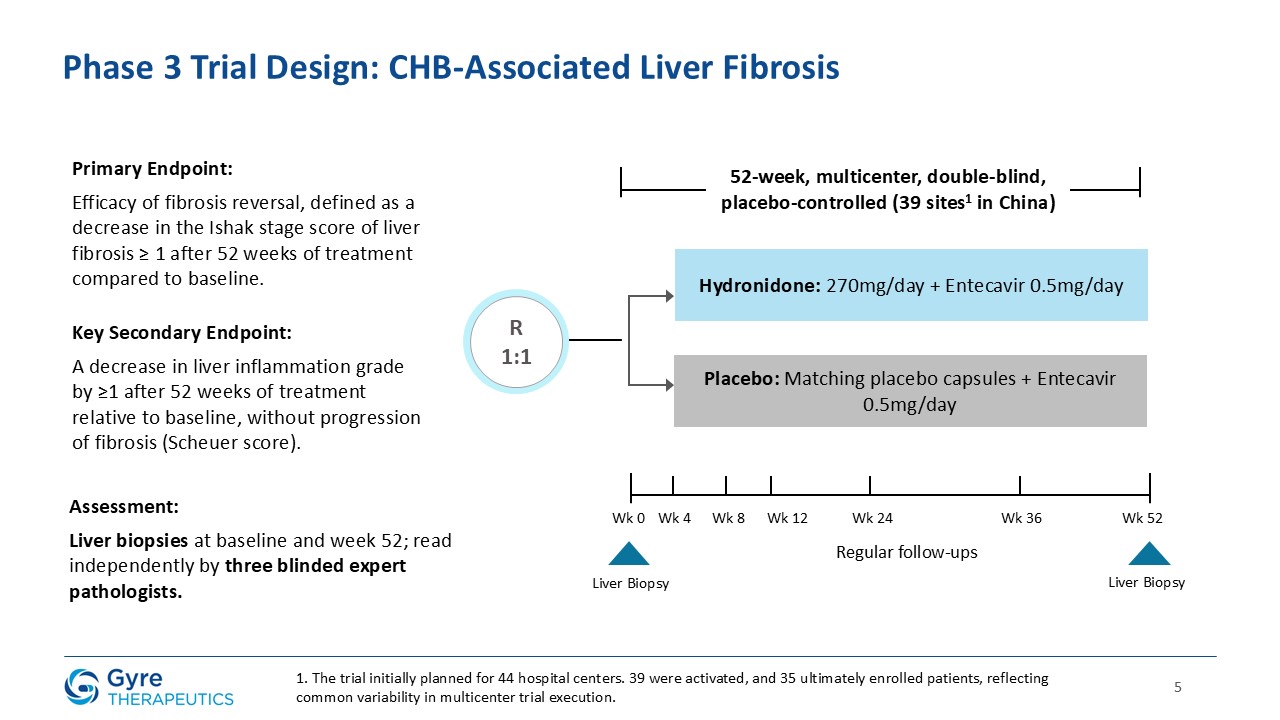
5 Hydronidone: 270mg/day + Entecavir 0.5mg/day Placebo: Matching placebo
capsules + Entecavir 0.5mg/day R1:1 Phase 3 Trial Design: CHB-Associated Liver Fibrosis 52-week, multicenter, double-blind, placebo-controlled (39 sites1 in China) Primary Endpoint: Efficacy of fibrosis reversal, defined as a decrease in
the Ishak stage score of liver fibrosis ≥ 1 after 52 weeks of treatment compared to baseline. Key Secondary Endpoint: A decrease in liver inflammation grade by ≥1 after 52 weeks of treatment relative to baseline, without progression of
fibrosis (Scheuer score). Assessment: Liver biopsies at baseline and week 52; read independently by three blinded expert pathologists. Wk 0 Wk 4 Wk 8 Wk 12 Wk 24 Wk 36 Wk 52 Regular follow-ups Liver Biopsy Liver Biopsy 1. The
trial initially planned for 44 hospital centers. 39 were activated, and 35 ultimately enrolled patients, reflecting common variability in multicenter trial execution.
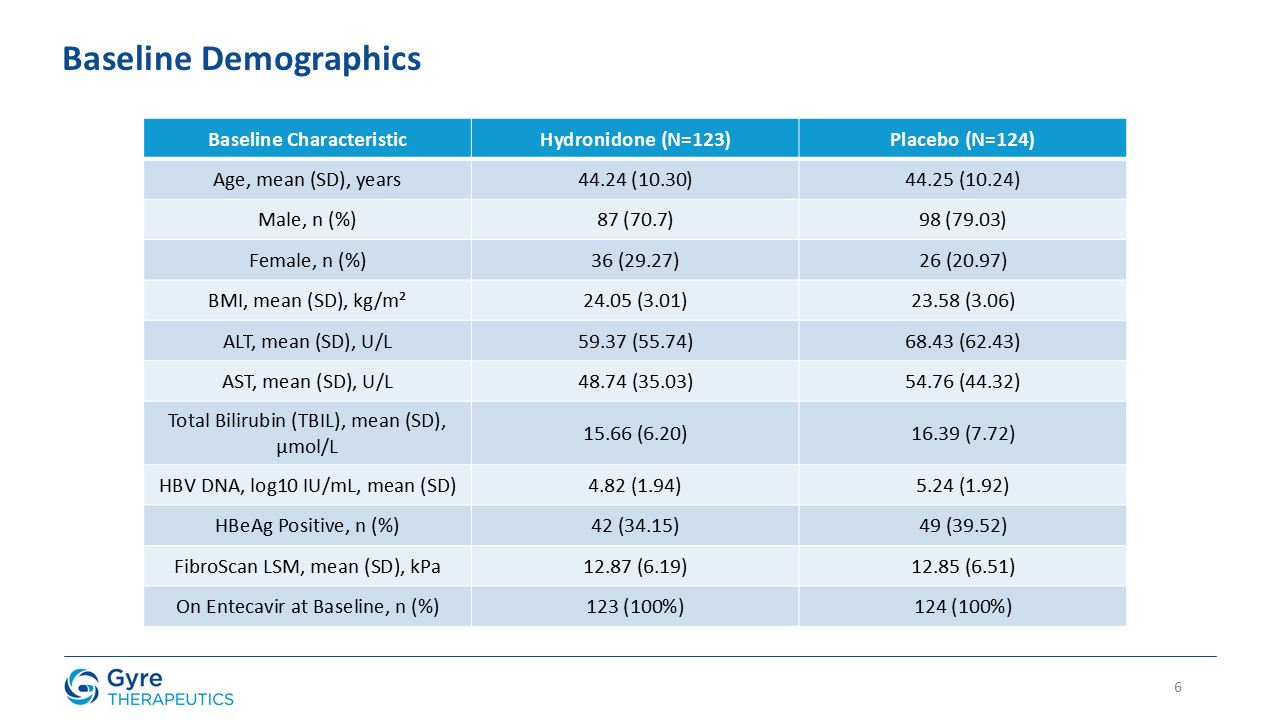
Baseline Characteristic Hydronidone (N=123) Placebo (N=124) Age, mean (SD),
years 44.24 (10.30) 44.25 (10.24) Male, n (%) 87 (70.7) 98 (79.03) Female, n (%) 36 (29.27) 26 (20.97) BMI, mean (SD), kg/m² 24.05 (3.01) 23.58 (3.06) ALT, mean (SD), U/L 59.37 (55.74) 68.43 (62.43) AST, mean (SD), U/L 48.74
(35.03) 54.76 (44.32) Total Bilirubin (TBIL), mean (SD), µmol/L 15.66 (6.20) 16.39 (7.72) HBV DNA, log10 IU/mL, mean (SD) 4.82 (1.94) 5.24 (1.92) HBeAg Positive, n (%) 42 (34.15) 49 (39.52) FibroScan LSM, mean (SD), kPa 12.87
(6.19) 12.85 (6.51) On Entecavir at Baseline, n (%) 123 (100%) 124 (100%) Baseline Demographics 6
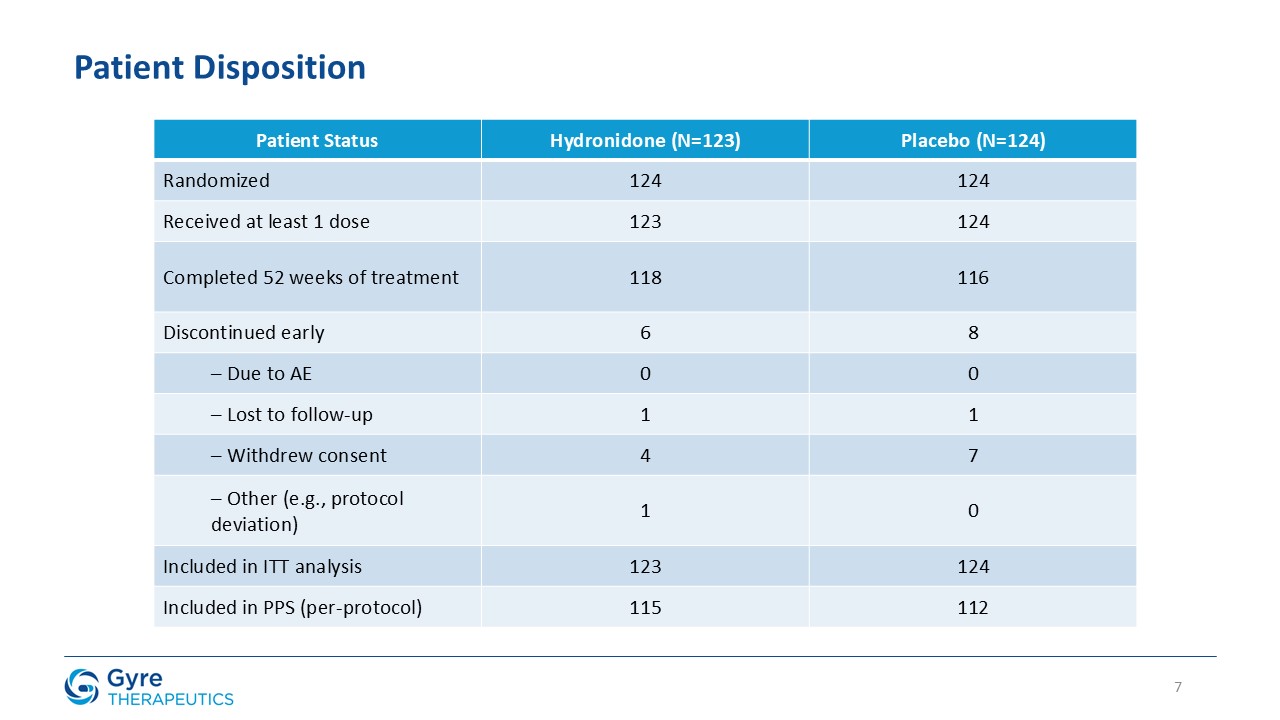
Patient Status Hydronidone (N=123) Placebo
(N=124) Randomized 124 124 Received at least 1 dose 123 124 Completed 52 weeks of treatment 118 116 Discontinued early 6 8 – Due to AE 0 0 – Lost to follow-up 1 1 – Withdrew consent 4 7 – Other (e.g., protocol
deviation) 1 0 Included in ITT analysis 123 124 Included in PPS (per-protocol) 115 112 Patient Disposition 7
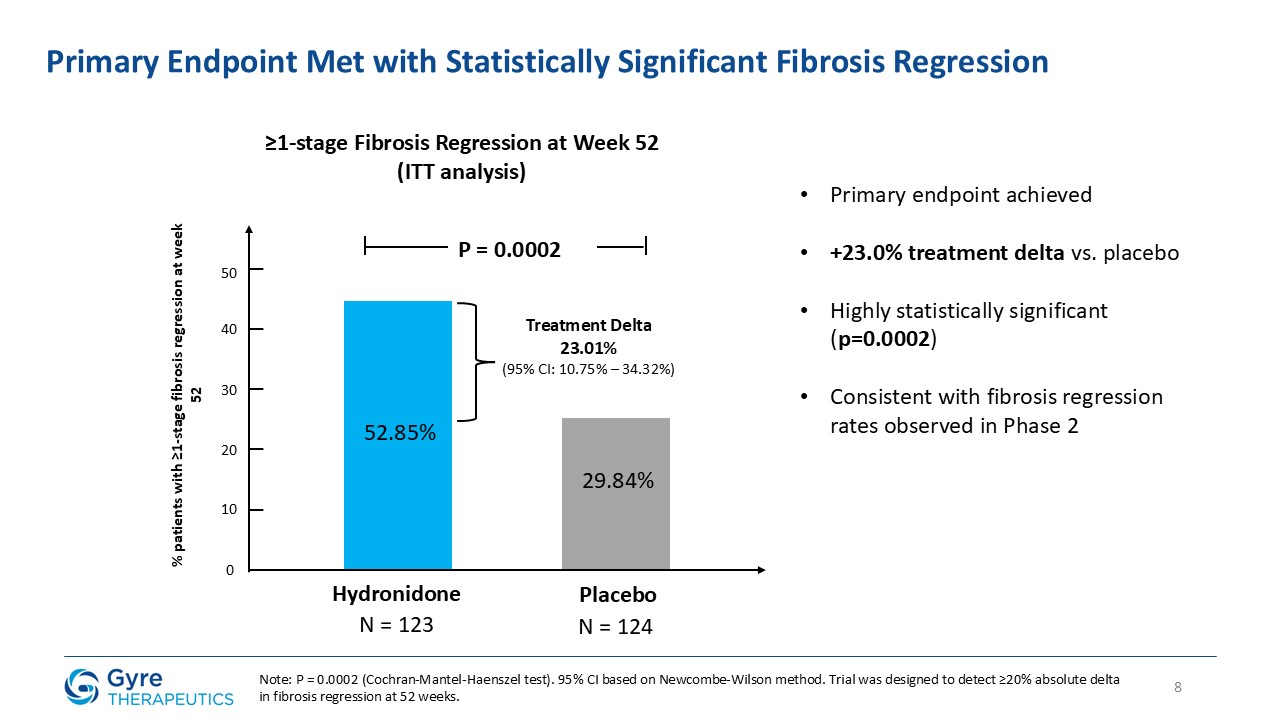
8 Primary Endpoint Met with Statistically Significant Fibrosis
Regression Hydronidone Placebo 52.85% 29.84% 0 10 P = 0.0002 % patients with ≥1-stage fibrosis regression at week 52 20 30 50 40 Treatment Delta 23.01% (95% CI: 10.75% – 34.32%) ≥1-stage Fibrosis Regression at Week 52 (ITT
analysis) N = 123 N = 124 Primary endpoint achieved +23.0% treatment delta vs. placebo Highly statistically significant (p=0.0002) Consistent with fibrosis regression rates observed in Phase 2 Note: P = 0.0002 (Cochran-Mantel-Haenszel
test). 95% CI based on Newcombe-Wilson method. Trial was designed to detect ≥20% absolute delta in fibrosis regression at 52 weeks.
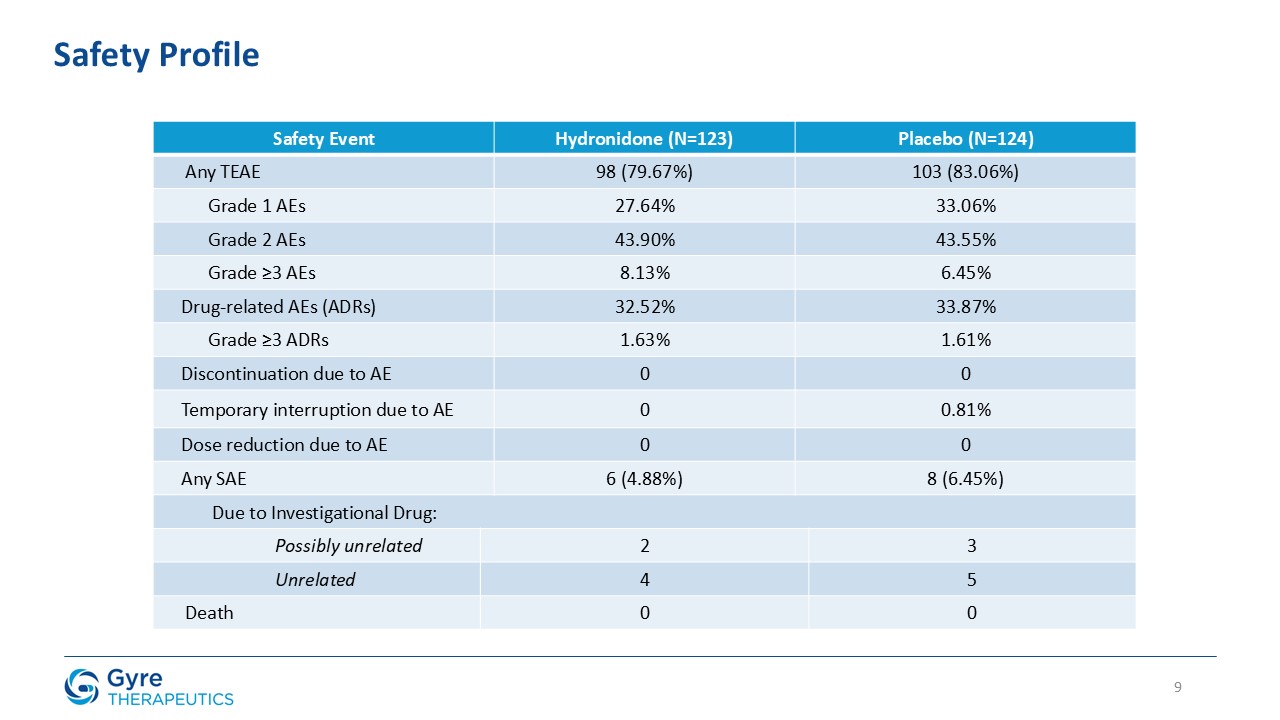
Safety Event Hydronidone (N=123) Hydronidone (N=123) Placebo (N=124) Placebo
(N=124) Any TEAE 98 (79.67%) 98 (79.67%) 103 (83.06%) 103 (83.06%) Grade 1 AEs 27.64% 27.64% 33.06% 33.06% Grade 2 AEs 43.90% 43.90% 43.55% 43.55% Grade ≥3 AEs 8.13% 8.13% 6.45% 6.45% Drug-related AEs
(ADRs) 32.52% 32.52% 33.87% 33.87% Grade ≥3 ADRs 1.63% 1.63% 1.61% 1.61% Discontinuation due to AE 0 0 0 0 Temporary interruption due to AE 0 0 0.81% 0.81% Dose reduction due to AE 0 0 0 0 Any SAE 6 (4.88%) 6
(4.88%) 8 (6.45%) 8 (6.45%) Due to Investigational Drug: Possibly unrelated 2 3 Unrelated 4 5 Death 0 0 Safety Profile 9
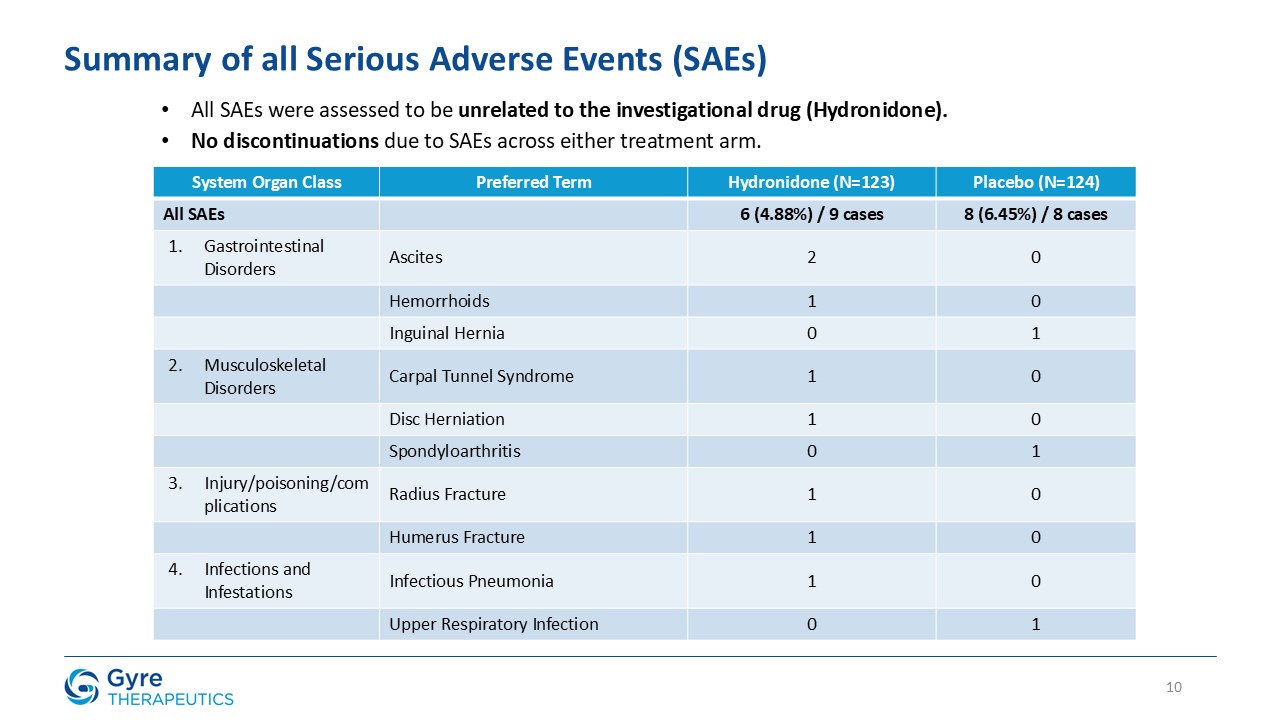
System Organ Class Preferred Term Hydronidone (N=123) Placebo (N=124) All
SAEs 6 (4.88%) / 9 cases 8 (6.45%) / 8 cases Gastrointestinal Disorders Ascites 2 0 Hemorrhoids 1 0 Inguinal Hernia 0 1 Musculoskeletal Disorders Carpal Tunnel Syndrome 1 0 Disc
Herniation 1 0 Spondyloarthritis 0 1 Injury/poisoning/complications Radius Fracture 1 0 Humerus Fracture 1 0 Infections and Infestations Infectious Pneumonia 1 0 Upper Respiratory Infection 0 1 All SAEs were assessed to be
unrelated to the investigational drug (Hydronidone). No discontinuations due to SAEs across either treatment arm. Summary of all Serious Adverse Events (SAEs) 10
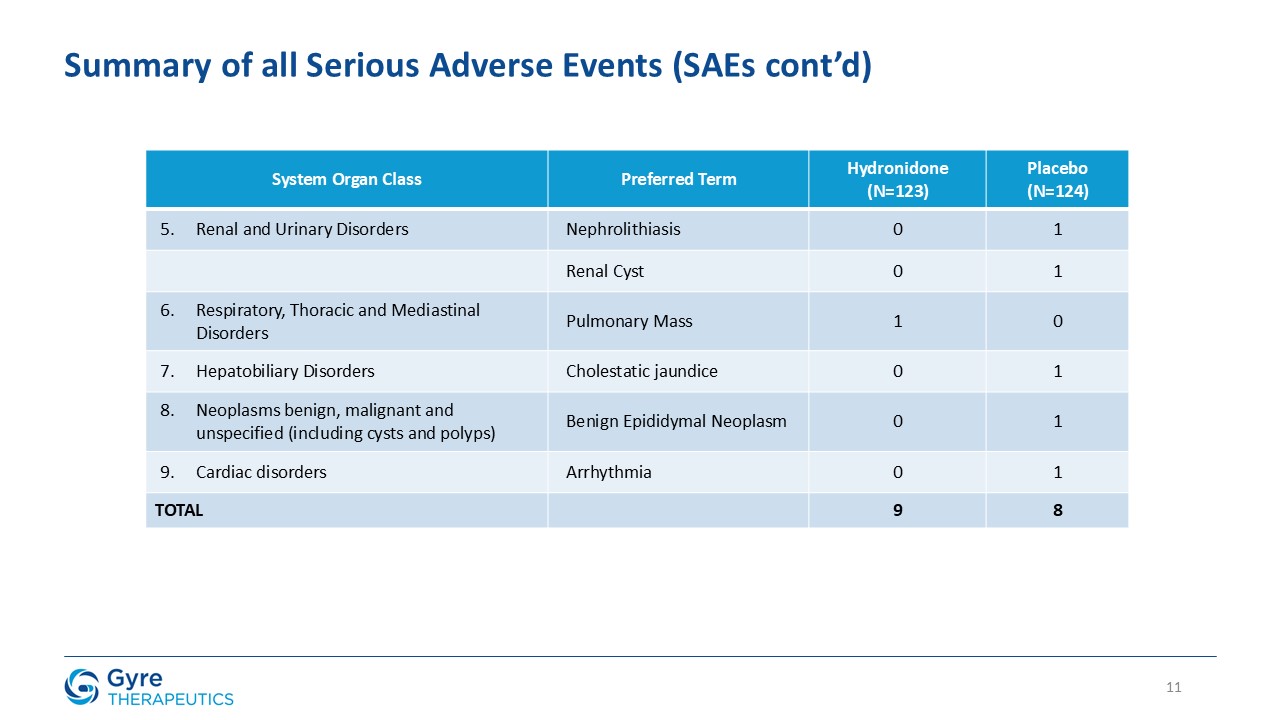
System Organ Class Preferred Term Hydronidone (N=123) Placebo (N=124) Renal
and Urinary Disorders Nephrolithiasis 0 1 Renal Cyst 0 1 Respiratory, Thoracic and Mediastinal Disorders Pulmonary Mass 1 0 Hepatobiliary Disorders Cholestatic jaundice 0 1 Neoplasms benign, malignant and unspecified
(including cysts and polyps) Benign Epididymal Neoplasm 0 1 Cardiac disorders Arrhythmia 0 1 TOTAL 9 8 Summary of all Serious Adverse Events (SAEs cont’d) 11
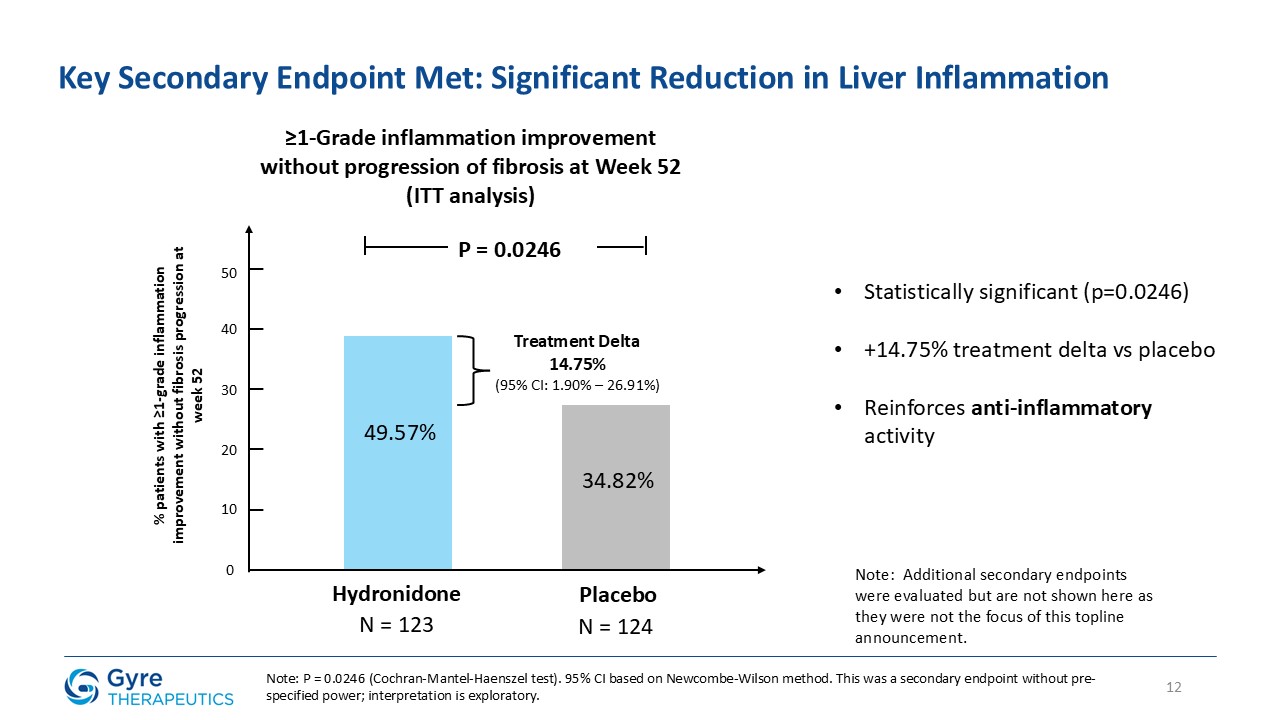
12 Key Secondary Endpoint Met: Significant Reduction in Liver
Inflammation Hydronidone Placebo 49.57% 34.82% 0 10 P = 0.0246 % patients with ≥1-grade inflammation improvement without fibrosis progression at week 52 20 30 50 40 Treatment Delta 14.75% (95% CI: 1.90% – 26.91%) ≥1-Grade
inflammation improvement without progression of fibrosis at Week 52 (ITT analysis) N = 123 N = 124 Statistically significant (p=0.0246) +14.75% treatment delta vs placebo Reinforces anti-inflammatory activity Note: Additional secondary
endpoints were evaluated but are not shown here as they were not the focus of this topline announcement. Note: P = 0.0246 (Cochran-Mantel-Haenszel test). 95% CI based on Newcombe-Wilson method. This was a secondary endpoint without
pre-specified power; interpretation is exploratory.
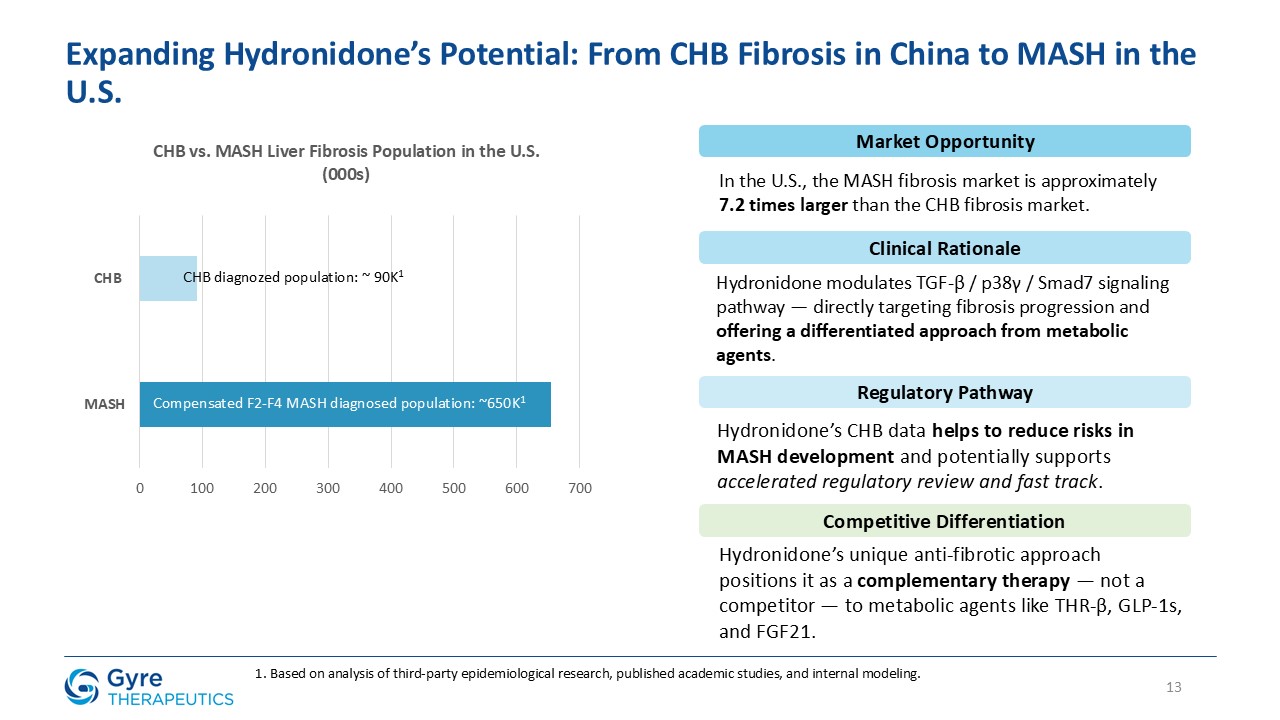
13 Expanding Hydronidone’s Potential: From CHB Fibrosis in China to MASH in the
U.S. 1. Based on analysis of third-party epidemiological research, published academic studies, and internal modeling. Compensated F2-F4 MASH diagnosed population: ~650K1 CHB diagnozed population: ~ 90K1 Market Opportunity In the U.S., the
MASH fibrosis market is approximately 7.2 times larger than the CHB fibrosis market. Clinical Rationale Hydronidone modulates TGF-β / p38γ / Smad7 signaling pathway — directly targeting fibrosis progression and offering a differentiated
approach from metabolic agents. Regulatory Pathway Hydronidone’s CHB data helps to reduce risks in MASH development and potentially supports accelerated regulatory review and fast track. Competitive Differentiation Hydronidone’s unique
anti-fibrotic approach positions it as a complementary therapy — not a competitor — to metabolic agents like THR-β, GLP-1s, and FGF21.
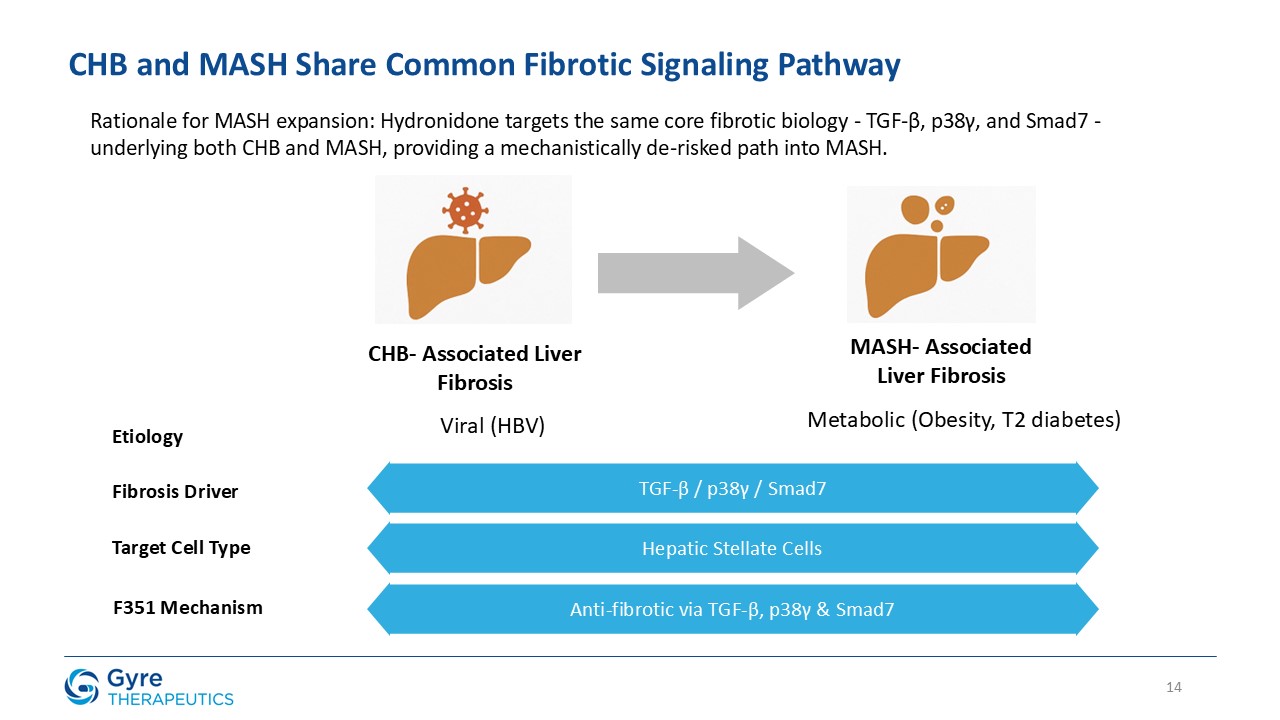
14 CHB and MASH Share Common Fibrotic Signaling Pathway CHB- Associated Liver
Fibrosis MASH- Associated Liver Fibrosis Etiology Viral (HBV) Metabolic (Obesity, T2 diabetes) Fibrosis Driver Target Cell Type F351 Mechanism TGF-β / p38γ / Smad7 Hepatic Stellate Cells Anti-fibrotic via TGF-β, p38γ &
Smad7 Rationale for MASH expansion: Hydronidone targets the same core fibrotic biology - TGF-β, p38γ, and Smad7 - underlying both CHB and MASH, providing a mechanistically de-risked path into MASH.
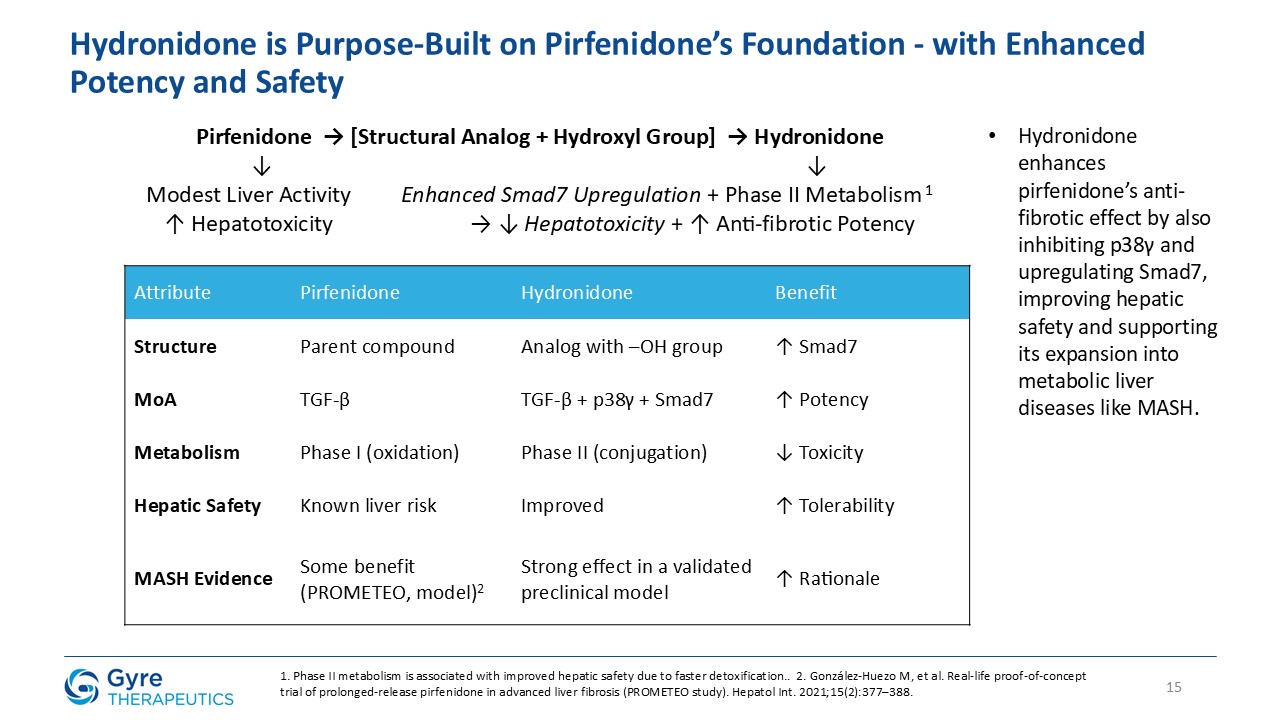
Hydronidone is Purpose-Built on Pirfenidone’s Foundation - with Enhanced Potency
and Safety 15 Pirfenidone → [Structural Analog + Hydroxyl Group] → Hydronidone ↓ ↓ Modest Liver Activity Enhanced Smad7 Upregulation + Phase II Metabolism 1 ↑ Hepatotoxicity → ↓ Hepatotoxicity + ↑ Anti-fibrotic
Potency Attribute Pirfenidone Hydronidone Benefit Structure Parent compound Analog with –OH group ↑ Smad7 MoA TGF-β TGF-β + p38γ + Smad7 ↑ Potency Metabolism Phase I (oxidation) Phase II (conjugation) ↓ Toxicity Hepatic
Safety Known liver risk Improved ↑ Tolerability MASH Evidence Some benefit (PROMETEO, model)2 Strong effect in a validated preclinical model ↑ Rationale 1. Phase II metabolism is associated with improved hepatic safety due to faster
detoxification.. 2. González-Huezo M, et al. Real-life proof-of-concept trial of prolonged-release pirfenidone in advanced liver fibrosis (PROMETEO study). Hepatol Int. 2021;15(2):377–388. Hydronidone enhances pirfenidone’s anti-fibrotic
effect by also inhibiting p38γ and upregulating Smad7, improving hepatic safety and supporting its expansion into metabolic liver diseases like MASH.
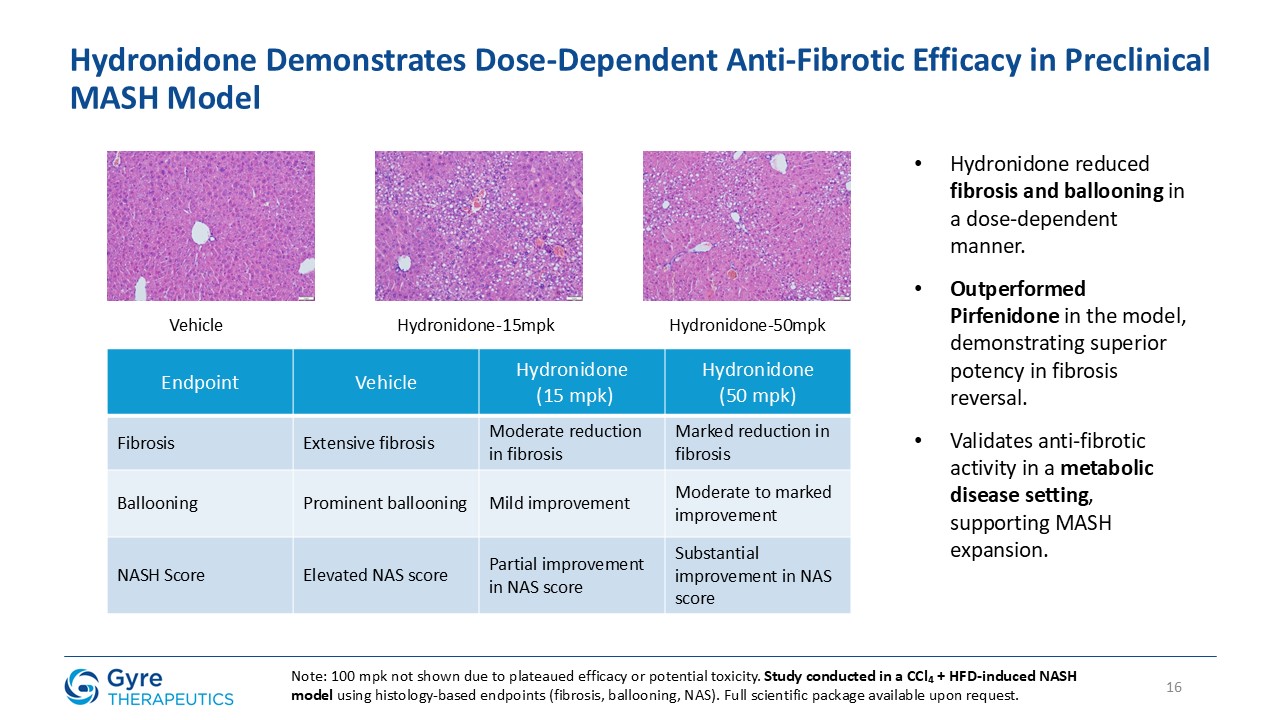
Hydronidone Demonstrates Dose-Dependent Anti-Fibrotic Efficacy in Preclinical MASH
Model 16 Vehicle Hydronidone-15mpk Hydronidone-50mpk Endpoint Vehicle Hydronidone (15 mpk) Hydronidone (50 mpk) Fibrosis Extensive fibrosis Moderate reduction in fibrosis Marked reduction in fibrosis Ballooning Prominent
ballooning Mild improvement Moderate to marked improvement NASH Score Elevated NAS score Partial improvement in NAS score Substantial improvement in NAS score Hydronidone reduced fibrosis and ballooning in a dose-dependent
manner. Outperformed Pirfenidone in the model, demonstrating superior potency in fibrosis reversal. Validates anti-fibrotic activity in a metabolic disease setting, supporting MASH expansion. Note: 100 mpk not shown due to plateaued efficacy
or potential toxicity. Study conducted in a CCl₄ + HFD-induced NASH model using histology-based endpoints (fibrosis, ballooning, NAS). Full scientific package available upon request.
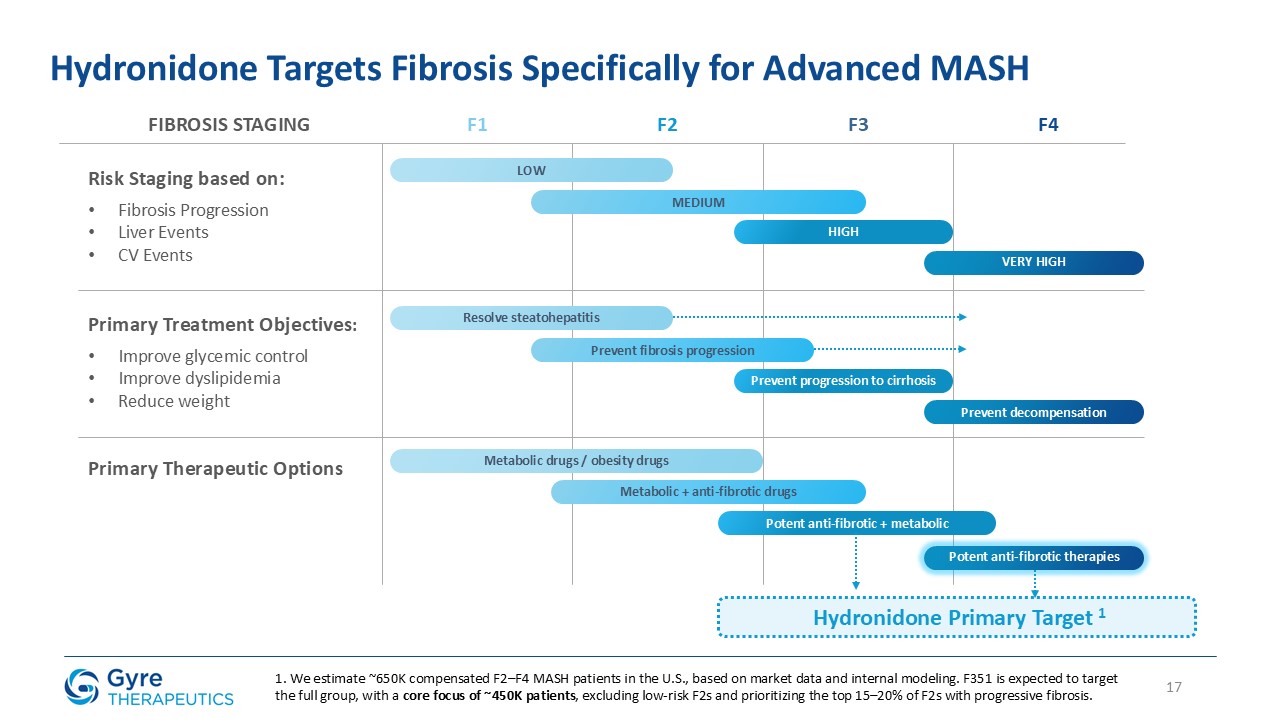
17 Hydronidone Targets Fibrosis Specifically for Advanced MASH FIBROSIS
STAGING Risk Staging based on: Fibrosis Progression Liver Events CV Events Primary Treatment Objectives: Improve glycemic control Improve dyslipidemia Reduce weight Primary Therapeutic Options F1 F2 F3 F4 LOW MEDIUM HIGH VERY
HIGH Resolve steatohepatitis Prevent fibrosis progression Prevent progression to cirrhosis Prevent decompensation Metabolic drugs / obesity drugs Metabolic + anti-fibrotic drugs Potent anti-fibrotic + metabolic Potent anti-fibrotic
therapies Hydronidone Primary Target 1 1. We estimate ~650K compensated F2–F4 MASH patients in the U.S., based on market data and internal modeling. F351 is expected to target the full group, with a core focus of ~450K patients, excluding
low-risk F2s and prioritizing the top 15–20% of F2s with progressive fibrosis.

Meaningful Fibrosis Regression Observed in Ishak 6
(F4) Patients in Two Independent Trials Subgroup-based analysis; not powered for statistical
significance.(Biopsy-confirmed results from 52-week, randomized, double-blind trials with blinded reads by independent pathologists) Phase 2:• 36% (5/14) of cirrhotic patients (Ishak 6) achieved ≥2-stage regression and were considered no longer cirrhotic at Week 52. •12/14 (86%) showed ≥1-stage improvement, indicating broad antifibrotic activity. •In the placebo arm, only 1 patient improved, which happened to be a ≥2-stage regression. Phase 3: •100%
(10/10) of cirrhotic patients (Ishak 6) in the treatment group had ≥1-stage regression at Week 52. •Mean
improvement was −1.5 vs. −1.0 in placebo. •Placebo response: 5/7 patients (71.4%) showed ≥1-stage regression, but
mean score change remained lower than Hydronidone. While exploratory and observed in CHB-associated cirrhosis, the
consistent ≥2-stage regression seen in Phase 2/3 suggests Hydronidone may have the potential to reverse cirrhosis.Note: Phase 2 and Phase 3 used different methods to assess fibrosis regression. Phase 2 reported categorical outcomes (including
≥2-stage regression), while Phase 3 focused on ≥1-stage improvement and mean Ishak score change. In both studies, analyses were limited to biopsy-confirmed cirrhotic patients (Ishak 6 at baseline) and evaluated fibrosis improvement at Week 52
separately from non-cirrhotic patients.

19 Positioning Hydronidone In The Evolving MASH Treatment
Landscape t ORAL INJECTABLE Hydronidone Rezdiffra VK2809 EFX Pegozafermin Tirzepatide Semaglutide Survodutide Indication CHB MASH MASH MASH MASH MASH MASH MASH Study Phase Phase 3 Approved Phase 2b Phase
2b Phase 2b Phase 2b Phase 2 Phase 2 MOA TGF-β THR-β THR-β FGF21 FGF21 GIP/GLP-1 GLP-1 GLP-1/glucagon Population ITT ITT ITT ITT ITT ITT ITT Modified ITT ITT N
(Active/Placebo) 123/124 ~319/~309 44/41 43/43 63/61 81/45 219/219 80/80 77/77 Total ITT 248 966 181 126 181 192 659 320 295 Focus F2 - F4 F2 - F3 F2 - F3 F2 - F3 F4 F2 - F3 F2 - F3 F2 - F3 F2 - F3 Duration 52
wks 52 wks 52 wks 96 wks 24 wks 52 wks 72 weeks 46 weeks Fibrosis
Improvement 52.9% ~26% 56.8% 49% 29% 27% 54.9% 43% 36% Placebo 29.8% ~10% 34.1% 19% 12% 7% 29.7% 33% 22% Placebo-Adjusted +23.0% +16% +22.7% +30% +17% +20% +25.2% +10% +14% Note: This illustrative comparison
includes data from distinct disease settings (CHB and MASH). While fibrosis is a shared endpoint, differences in etiology, pathophysiology, and trial design limit direct comparability. Cross-indication interpretation is hypothetical and does
not imply therapeutic equivalence. Rezdiffra (Madrigal) sets the benchmark as the first FDA-approved therapy for MASH. Hydronidone offers a fibrosis-first approach, acting directly on fibrotic tissue, and is the only agent with a demonstrated
focus on F4 (cirrhotic) patients. Hydronidone is designed to be complementary, not competitive — potentially used as an add-on alongside metabolic agents. Our regulatory aim is to establish a new standard for direct fibrosis reversal in MASH
patients. Comparator data sourced from published studies and company press releases (e.g., Madrigal, Viking, Akero, 89bio, Lilly, Novo Nordisk, Boehringer Ingelheim). Differences in disease, design, and population limit direct comparison.
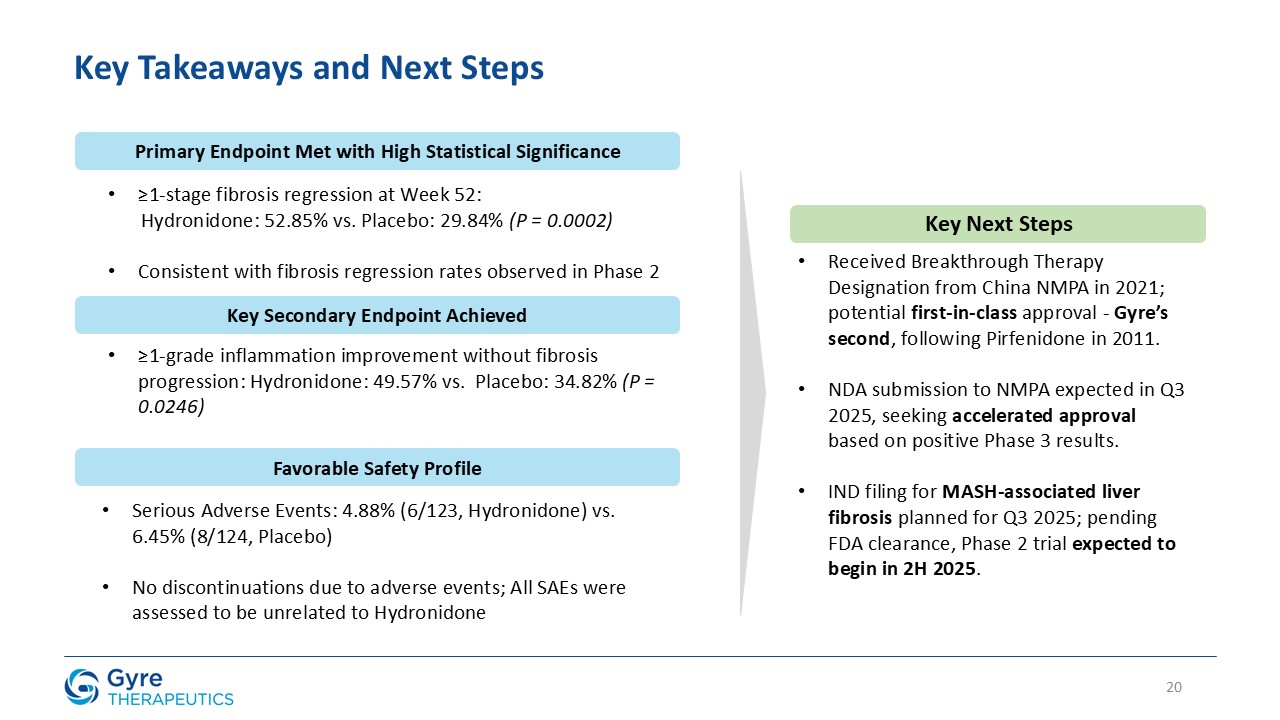
20 Key Takeaways and Next Steps Primary Endpoint Met with High Statistical
Significance ≥1-stage fibrosis regression at Week 52: Hydronidone: 52.85% vs. Placebo: 29.84% (P = 0.0002) Consistent with fibrosis regression rates observed in Phase 2 Key Secondary Endpoint Achieved ≥1-grade inflammation improvement
without fibrosis progression: Hydronidone: 49.57% vs. Placebo: 34.82% (P = 0.0246) Reinforces anti-inflammatory activity Favorable Safety Profile Serious Adverse Events: 4.88% (6/123, Hydronidone) vs. 6.45% (8/124, Placebo) No
discontinuations due to adverse events; All SAEs were assessed to be unrelated to Hydronidone Key Next Steps Received Breakthrough Therapy Designation from China NMPA in 2021; potential first-in-class approval - Gyre’s second, following
Pirfenidone in 2011. NDA submission to NMPA expected in Q3 2025, seeking accelerated approval based on positive Phase 3 results. IND filing for MASH-associated liver fibrosis planned for Q3 2025; pending FDA clearance, Phase 2 trial expected
to begin in 2H 2025.
21 APPENDIX: Clinical Trial - Common Adverse Events Detail & F351 -
Mechanism of Action
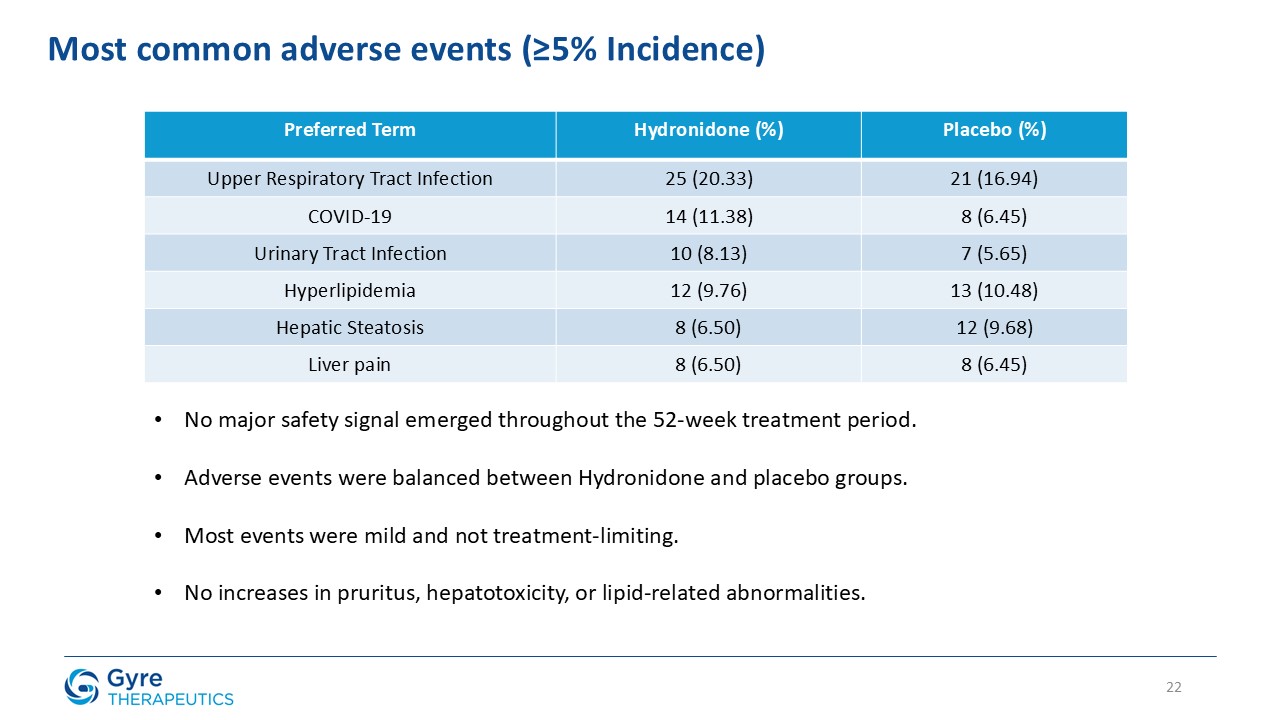
Preferred Term Hydronidone (%) Placebo (%) Upper Respiratory Tract
Infection 25 (20.33) 21 (16.94) COVID-19 14 (11.38) 8 (6.45) Urinary Tract Infection 10 (8.13) 7 (5.65) Hyperlipidemia 12 (9.76) 13 (10.48) Hepatic Steatosis 8 (6.50) 12 (9.68) Liver pain 8 (6.50) 8 (6.45) 22 Most common
adverse events (≥5% Incidence) No major safety signal emerged throughout the 52-week treatment period. Adverse events were balanced between Hydronidone and placebo groups. Most events were mild and not treatment-limiting. No increases in
pruritus, hepatotoxicity, or lipid-related abnormalities.
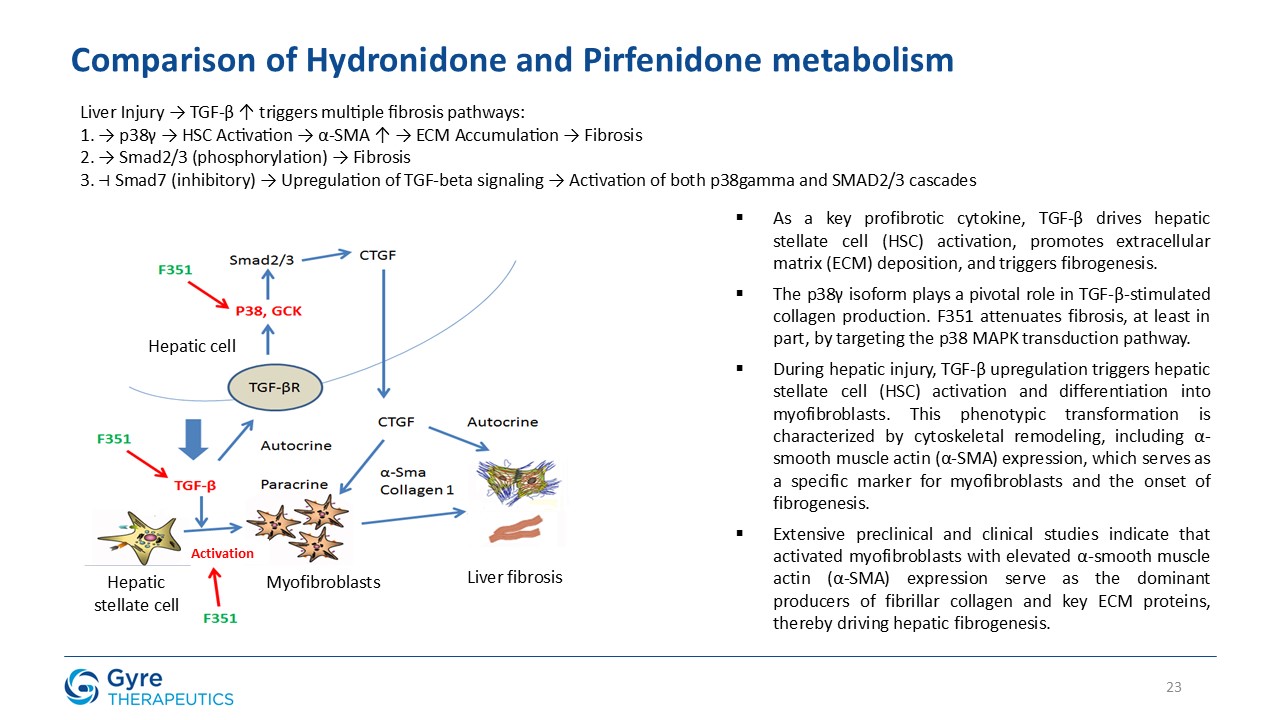
23 Comparison of Hydronidone and Pirfenidone metabolism Hepatic cell Hepatic
stellate cell Myofibroblasts Liver fibrosis Activation As a key profibrotic cytokine, TGF-β drives hepatic stellate cell (HSC) activation, promotes extracellular matrix (ECM) deposition, and triggers fibrogenesis. The p38γ isoform plays a
pivotal role in TGF-β-stimulated collagen production. F351 attenuates fibrosis, at least in part, by targeting the p38 MAPK transduction pathway. During hepatic injury, TGF-β upregulation triggers hepatic stellate cell (HSC) activation and
differentiation into myofibroblasts. This phenotypic transformation is characterized by cytoskeletal remodeling, including α-smooth muscle actin (α-SMA) expression, which serves as a specific marker for myofibroblasts and the onset of
fibrogenesis. Extensive preclinical and clinical studies indicate that activated myofibroblasts with elevated α-smooth muscle actin (α-SMA) expression serve as the dominant producers of fibrillar collagen and key ECM proteins, thereby driving
hepatic fibrogenesis. Liver Injury → TGF-β ↑ triggers multiple fibrosis pathways: 1. → p38γ → HSC Activation → α-SMA ↑ → ECM Accumulation → Fibrosis 2. → Smad2/3 (phosphorylation) → Fibrosis 3. ⊣ Smad7 (inhibitory) → Upregulation of TGF-beta
signaling → Activation of both p38gamma and SMAD2/3 cascades
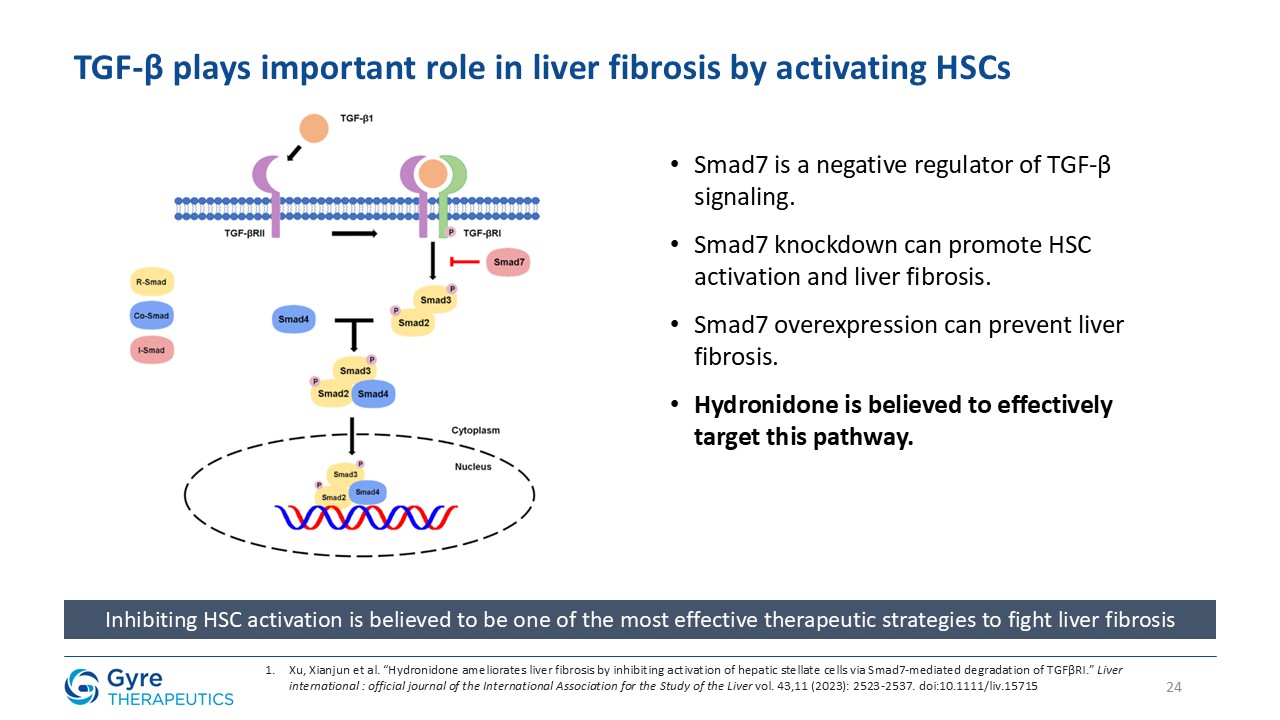
Smad7 is a negative regulator of TGF-β signaling. Smad7 knockdown can promote HSC
activation and liver fibrosis. Smad7 overexpression can prevent liver fibrosis. Hydronidone is believed to effectively target this pathway. Inhibiting HSC activation is believed to be one of the most effective therapeutic strategies to fight
liver fibrosis 24 Xu, Xianjun et al. “Hydronidone ameliorates liver fibrosis by inhibiting activation of hepatic stellate cells via Smad7-mediated degradation of TGFβRI.” Liver international : official journal of the International Association
for the Study of the Liver vol. 43,11 (2023): 2523-2537. doi:10.1111/liv.15715 TGF-β plays important role in liver fibrosis by activating HSCs
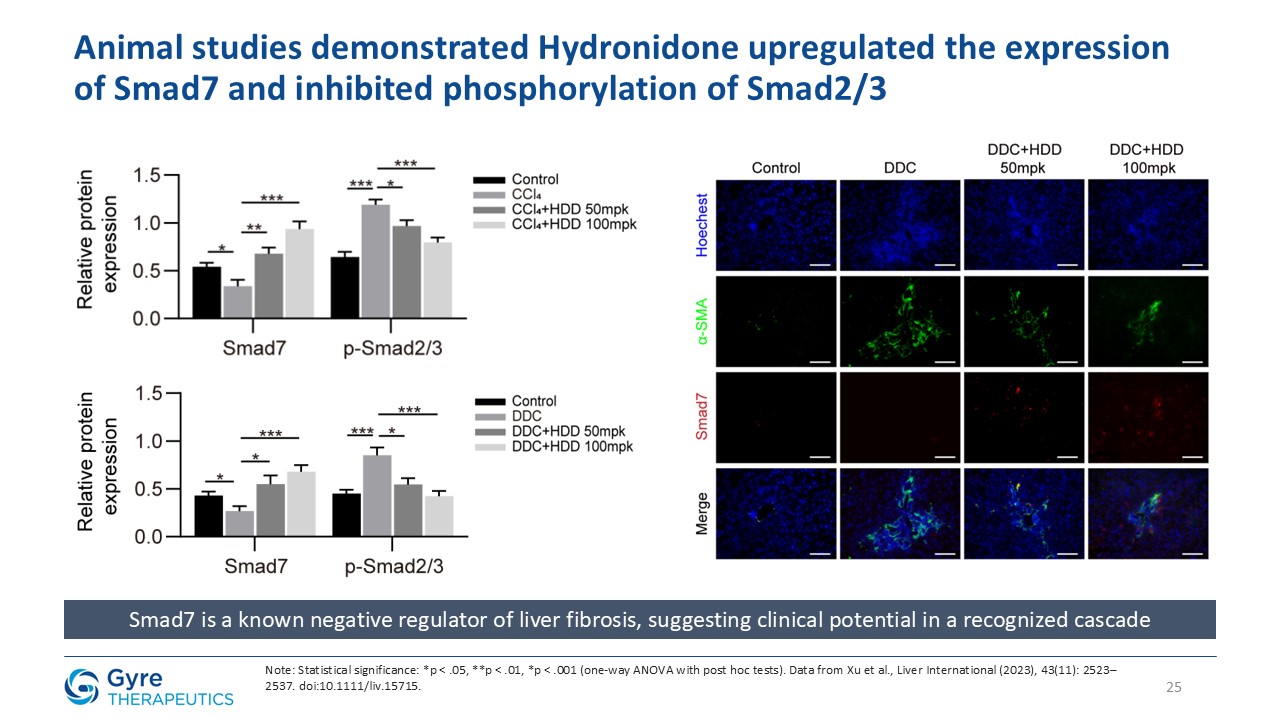
Smad7 is a known negative regulator of liver fibrosis, suggesting clinical
potential in a recognized cascade Note: Statistical significance: *p < .05, **p < .01, *p < .001 (one-way ANOVA with post hoc tests). Data from Xu et al., Liver International (2023), 43(11): 2523–2537.
doi:10.1111/liv.15715. 25 Animal studies demonstrated Hydronidone upregulated the expression of Smad7 and inhibited phosphorylation of Smad2/3

26 Hydronidone vs. Pirfenidone: Mechanistic and safety advantages The
introduction of a hydroxyl group shifts its metabolic profile from Pirfenidone’s dominant Phase I oxidation to preferential Phase II conjugation (M3/M4 metabolites). Phase II metabolism, known as “detoxification metabolism,” can prevent the
formation of active metabolites and covalent binding to proteins, suggesting a mechanistic basis for hydronidone’s improved hepatic safety profile compared with Pirfenidone. Phase II metabolism Phase I metabolism Optimization Achieve higher
P38γ binding affinity Pirfenidone Hydronidone Kinase Inhibition Profile In vitro kinase assay shows that both hydronidone and Pirfenidone effectively inhibit p38γ activity, with hydronidone exhibiting a higher inhibition potency than
Pirfenidone. These findings indicate that hydronidone exhibits stronger inhibition of the p38γ pathway, potentially contributing to its enhanced antifibrotic activity.
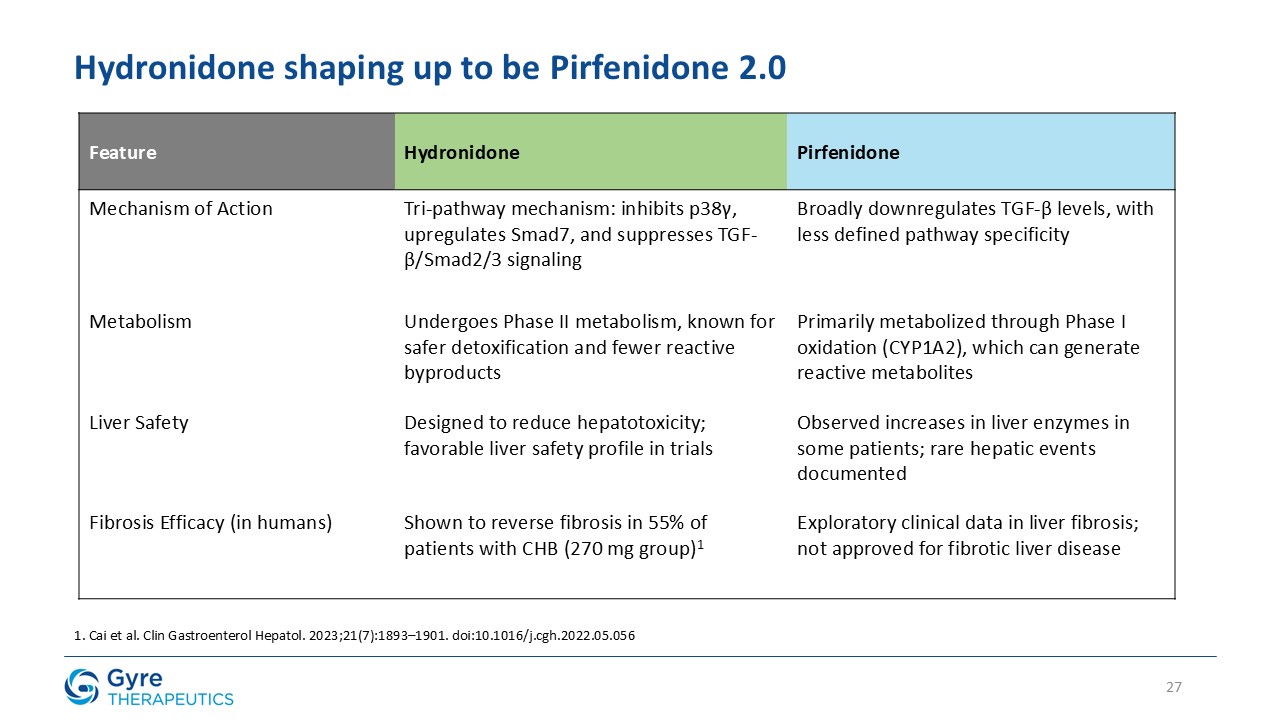
27 Hydronidone shaping up to be Pirfenidone
2.0 Feature Hydronidone Pirfenidone Mechanism of Action Tri-pathway mechanism: inhibits p38γ, upregulates Smad7, and suppresses TGF-β/Smad2/3 signaling Broadly downregulates TGF-β levels, with less defined pathway
specificity Metabolism Undergoes Phase II metabolism, known for safer detoxification and fewer reactive byproducts Primarily metabolized through Phase I oxidation (CYP1A2), which can generate reactive metabolites Liver Safety Designed to
reduce hepatotoxicity; favorable liver safety profile in trials Observed increases in liver enzymes in some patients; rare hepatic events documented Fibrosis Efficacy (in humans) Shown to reverse fibrosis in 55% of patients with CHB (270 mg
group)1 Exploratory clinical data in liver fibrosis; not approved for fibrotic liver disease 1. Cai et al. Clin Gastroenterol Hepatol. 2023;21(7):1893–1901. doi:10.1016/j.cgh.2022.05.056

28 Thank you Contact: David Zhang David.Zhang@Gyretx.com